Reproductive System and the Embryonic Development
The reproductive system produces the sex cells and sex hormones with the female system supporting the developing embryo and producing milk. Let’s review the basic concepts related to the reproductive system.
Table of Contents
- Reproduction: The Creation of New Life
- The Human Reproductive System
- The Creation of Gametes: Gametogenesis
- The Female Reproductive Cycle
- Effects of Pregnancy and Contraceptives
- Diseases of the Reproductive System
- Embryonic Development
- Overview of Human Development
- Download Article in PDF Format
- Test Yourself!
Reproduction: The Creation of New Life
The creation of new individuals from existing ones is reproduction. In a way, this allows species to transcend time whereas an individual in the species can only exist for a relatively short life span. As mentioned before, organisms can either reproduce asexually or sexually and we will focus more on sexual reproduction.
Sexual reproduction is the creation of offspring through the process of fertilization, the union of sperm and egg. Both types of cells, called gametes, contain chromosomes. The sperm is a relatively small cell that moves through its flagellum while the egg is a much larger, non-propelling cell. When eggs and sperm unite, a diploid zygote is formed. This zygote develops into a new individual while containing a unique combination of genes inherited from its parents.

Although sexual reproduction has advantages, it presents a problem for nonmobile animals or those that live solitary lives: finding a mate. One solution for them is through hermaphroditism, that is each individual has both male and female reproductive systems. Some can fertilize their own eggs while others require a partner, with both organs donating and receiving sperm during mating.
The mechanism of fertilization plays a key role in sexual reproduction. Most aquatic animals and also amphibians exhibit external fertilization where the parents discharge their gametes into the environment often, without the need for either male or female to make contact. Timing is crucial for this mode of fertilization but in other species, specific courtship behavior is developed before the release of gametes can occur. In contrast, internal fertilization occurs when the sperm are deposited into or near the female and the gametes end up ultimately uniting within the female.
You already know the drill! We will now take a closer look at the human reproductive systems.
The Human Reproductive System
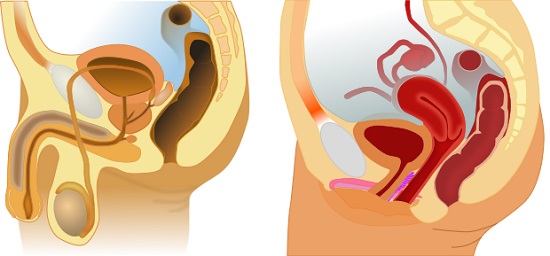
Although there are anatomical differences between the male and female reproductive systems, there are some important similarities. Both sexes have a gonad, organs which produce gametes. Both sexes have ducts that store and deliver those gametes, and also structures that allow mating.
1. The Female Reproductive System
A woman’s gonads, her ovaries, have a bumpy surface which is created by follicles that contain one developing egg, surrounded by cells that nourish and protect it. These follicle cells also produce the female sex hormone estrogen. A female has 1-2 million follicles at birth but will only release several hundred egg cells during her reproductive years. At puberty, one follicle matures and releases an immature egg cell about every 28 days in a process called ovulation. This continues until a woman reaches menopause.
After ovulation, what is left of the follicle grows in the ovary forming a mass of endocrine tissue called the corpus luteum which secretes additional estrogen, as well as progesterone, a hormone that helps maintain the uterine lining during pregnancy. If the released egg isn’t fertilized, the corpus luteum degenerates, and a new follicle matures during the next cycle.
Each ovary lies next to the opening of an oviduct, also known as the fallopian tubes. The ovary is actually separated from the fallopian tubes by a tiny space and during ovulation, the egg passes through this space into the oviduct where cilia sweep it to the uterus. If there is sperm, fertilization occurs here in the fallopian tubes. The resulting zygote starts to divide and become an embryo, as it moves along the oviduct.
The uterus or the womb is the site of pregnancy. It has a thick muscular wall, and its inner lining, the endometrium, is supplied with many blood vessels. An embryo is able to continue developing when it implants in this lining. The term embryo refers to the stage in development from the first division of the zygote until body structures begin to appear (about 8 weeks after fertilization in humans), after which it is called a fetus until birth.
The uterus is the normal site of pregnancy but sometimes, the embryo implants somewhere else in a condition known as ectopic pregnancy, most cases of which occur when the embryo implants in the oviduct or sometimes the outside walls of the uterus. In which case, it requires medical intervention.
The narrow neck at the bottom of the uterus is the cervix, which opens into the vagina. The latter is a thin-walled but strong muscular chamber that serves as the birth canal through which the baby is born. This is also the site where the sperm is deposited during intercourse. Glands in the organ secrete mucus which facilitates the process of depositing sperm.
The collective term for the external female genitalia is called the vulva. A pair of lighter skin folds, the labia minora border the openings of the vagina while the thicker skin folds, the labia majora, protect the vaginal opening. A thin piece of tissue called the hymen partly covers the vaginal opening until intercourse or vigorous sexual activity ruptures it. The vagina, labia minora, and a small erectile organ called the clitoris all engorge with blood and enlarge during sexual activity.
Now that we’ve learned the structures that make up the female reproductive system, we’ll examine the structures of the male reproductive system next.
2. The Male Reproductive System
The male gonads, or testes, are housed in a sac called the scrotum. A testis within a scrotum is called a testicle. In humans, sperm cannot develop optimally at core body temperature. The scrotum keeps the sperm cells about two degrees Celsius cooler for them to function normally. In the cold, the muscles around the scrotum contract and pull the testes toward the body, increasing and helping maintain the proper temperature for sperm cells.
From each testis, sperm cells pass into a coiled tube called the epididymis which stores the sperm as they develop. Sperm leaves this organ during ejaculation, the expulsion of sperm-containing fluid from the penis. During ejaculation, muscular contractions propel the sperm from the epididymis to another duct, the vas deferens. The vas deferens passes upward into the abdomen and loops around the urinary bladder.
Next to the bladder, the vas deferens joins a short duct from a gland, the seminal vesicle. These two ducts unite into a short ejaculatory duct where the sperm from the other testis enters. The duct empties into the urethra, which conveys (at different times) urine or sperm out through the penis. Thus, unlike females, there is a direct connection between the male reproductive and urinary systems.
In addition to the testes and ducts, the male reproductive system contains three sets of glands: the seminal vesicles, the prostate gland, and the bulbourethral glands. The seminal vesicles secrete a thick fluid containing mucus and fructose, which provides most of the energy used by the sperm as they propel themselves through the female reproductive tract.
The prostate secretes a thin, milky fluid that further nourishes the sperm. The bulbourethral glands (otherwise known as Cowper’s glands) secrete a clear alkaline mucus which may carry some sperm; this is one reason why the withdrawal of the penis before ejaculation isn’t guaranteed method of birth control.
Together, the sperm and the secretions of the glands make up semen which is discharged in a series of rhythmic, involuntary contractions of the reproductive structures during orgasm. The alkalinity of the semen balances the acidity and any traces of urine in the urethra while neutralizing the acidic environment of the vagina, protecting the sperm, and increasing their motility.
The penis consists mainly of erectile tissue and like the clitoris, it has shafts that support the sensitive glans or head. A fold of skin called the prepuce or foreskin covers the glans and this is removed through the process of circumcision.
The erectile tissue is made of modified veins and capillaries that fill with blood supplied by arteries during sexual arousal. Erection is essential for inserting and depositing sperm into the vagina during intercourse. Erectile dysfunction (ED) or impotence is the inability to achieve an erection.
Hormones from the hypothalamus and pituitary gland control the production of sperm by the testes. Not only that of the sperm but also the eggs in females. The creation of gametes will be covered in our next article in this series.
The Creation of Gametes: Gametogenesis
The creation of sperm (or spermatogenesis) and the egg (or oogenesis) is significantly different and must be examined separately.
1. Spermatogenesis.
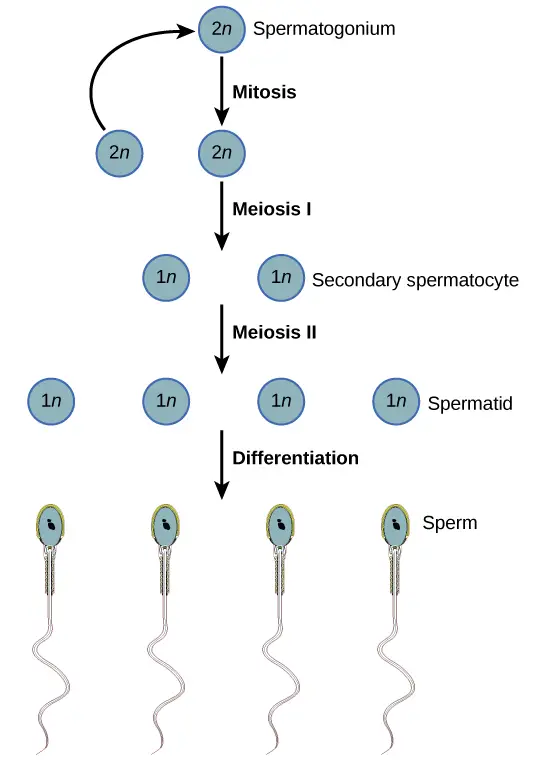
Sperm develop in the testes in coiled tubes known as the seminiferous tubules. Diploid cells are found near the outside wall of the tubules and multiply continuously by mitosis and differentiate into primary spermatocytes. Meiosis I of primary spermatocytes produces secondary spermatocytes and each has haploid chromosomes. Meiosis II then forms four cells (still haploid).
A sperm cell develops by the differentiation of each cell, pushing towards the center of the seminiferous tubules. From there, it is passed to the epididymis where it matures, becomes motile, and is stored.
2. Oogenesis
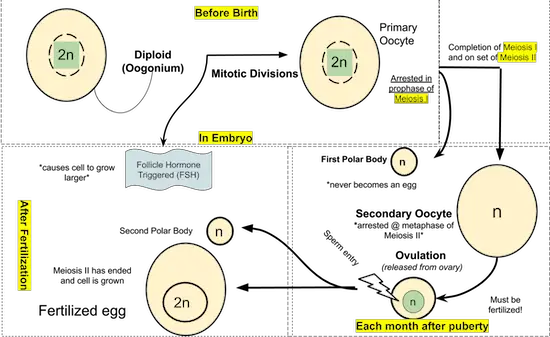
Most stages of oogenesis occur in the ovary. It begins prior to birth; in the womb, a female fetus will have developing follicles that begin meiosis. At birth, each follicle contains dormant primary oocytes, a diploid cell resting in the prophase of meiosis I. This primary oocyte is triggered by hormones to develop further during puberty.
The follicle-stimulating hormone (FSH) from the pituitary causes the follicles to enlarge and the primary oocyte to complete meiosis I and begin meiosis II, halting at metaphase II. The division of the cytoplasm in meiosis I is unequal, with a single secondary oocyte receiving almost all of it. The smaller of the two oocytes, the first polar body, receives almost no cytoplasm.
The secondary oocyte is released by the ovary during ovulation. It goes to the oviduct and if sperm fertilizes it, the secondary oocyte completes meiosis II. Meiosis II is also unequal, creating a second polar body and a mature egg. The nucleus of the mature egg can fuse with the nucleus of the sperm cell, producing the zygote.
Comparing Spermatogenesis and Oogenesis
Oogenesis and spermatogenesis are similar in that they produce haploid gametes. However, three important differences are highlighted between the two. The first is the number of gametes produced by each. In oogenesis, only one mature egg results from the diploid cell that undergoes meiosis. The other products, the polar bodies, degenerate. Whereas in spermatogenesis, all four products of meiosis develop into mature gametes.
Second, spermatogenesis continues from puberty until death while in oogenesis, mitotic divisions are thought to be completed before birth and the production of mature gametes ends at menopause.
Third, oogenesis has long “resting” periods whereas spermatogenesis is usually an uninterrupted sequence.
It seems that the female reproductive system has more intricate systems in place with regards to creating an egg. The regulation of such processes will be examined next.
The Female Reproductive Cycle
Females have a recurring sequence of events that produces gametes, makes them available for fertilization and prepares the body for pregnancy. This cycle repeats about every 28 days on average, but cycles from 20 to 40 days are not uncommon.
This cycle is actually two closely linked cycles: the ovarian cycle which controls oogenesis and the menstrual cycle which prepares the uterus for possible implantation of an embryo. Hormones coordinate these two cycles and the growing embryo and we will take a view of these cycles.
Overview of Ovarian and Menstrual Cycles
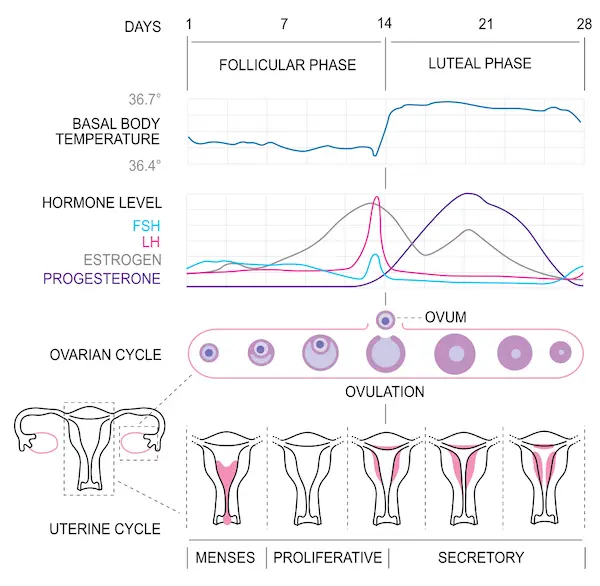
For simplicity, we will divide the ovarian cycle into two phases separated by ovulation: pre-ovulation, when a follicle is growing and a secondary oocyte is developing; and post-ovulation, where the follicle becomes a corpus luteum.
The menstrual cycle synchronizes with the ovarian cycle and by convention, the first day of a woman’s period is designated as the first day of the menstrual cycle. Menstruation is the bleeding caused by the breakdown of the endometrium. This also corresponds with the pre-ovulation phase of the ovarian cycle.
After menstruation, the endometrium grows. It continues to thicken throughout ovulation and if an embryo isn’t implanted in the uterine lining, menstruation begins again, marking the start of the next ovarian and menstrual cycles.
Hormones synchronize the events in the ovarian cycle with the menstrual cycle. A releasing hormone from the hypothalamus regulates the secretion of two pituitary hormones: FSH (Follicle-stimulating hormone) and LH (Luteinizing hormone). Changes in FSH and LH in the blood, as well as those of estrogen and progesterone, coincide with specific events in the ovarian and menstrual cycles.
Hormones Before Ovulation
The releasing hormone from the hypothalamus stimulates the anterior pituitary to increase FSH and LH. FSH stimulates the growth of ovarian follicles, starting the ovarian cycle. In turn, the follicles secrete estrogen, and more estrogen is secreted as the follicle grows.
The estrogen level is still very low and exerts negative feedback on the pituitary, maintaining a low level of FSH and LH in the blood, pre-ovulation. As ovulation nears, hormone levels change with estrogen increasing to a critical peak and creating positive feedback on the hypothalamus, leading to surges in FSH and LH.
Hormones During and After Ovulation
LH stimulates the completion of meiosis I, turning the primary oocyte into a secondary oocyte in the follicle. It also signals enzymes to rupture the follicle, releasing the oocyte and triggering the development of the corpus luteum from the ruptured follicle (hence the name luteinizing hormone). LH also promotes the secretion of progesterone and estrogen by the corpus luteum.
High levels of estrogen and progesterone in the blood following ovulation have influences on both the ovary and uterus. The combination of the two hormones creates negative feedback on the hypothalamus and pituitary, dropping the FSH and LH levels. This drop prevents follicles from developing and ovulation from occurring after an oocyte is already released.
The drop in LH is followed by the gradual degeneration of the corpus luteum. Near the end of the post-ovulation phase, unless an embryo gets implanted in the uterus, the corpus luteum stops secreting estrogen and progesterone. As blood levels of the two hormones decline, the hypothalamus can once again stimulate the pituitary to secrete more FSH and LH, and a new cycle begins.
Control of the Menstrual Cycle
Hormone control of the menstrual cycle is simpler than that of the ovarian cycle as it is regulated by estrogen and progesterone alone. The endometrium thickens in response to rising levels of estrogen and, later, progesterone. When levels of these hormones fall, the endometrium sheds leading to menstrual bleeding.
Because hormones play a role in the different reproductive cycles of women, they also affect how pregnancy develops. This is also the reason why contraceptives work in preventing unwanted pregnancies.
Effects of Pregnancy and Contraceptives
After ovulation, if an embryo is implanted in the uterus, the ovarian and menstrual cycles are put on hold. The developing embryo, within the endometrium, releases the hormone human chorionic gonadotropin (hCG) which maintains the corpus luteum and its function of secreting progesterone and estrogen. This keeps the endometrium intact and is also the hormone detected by pregnancy tests.
The steady levels of hormones during pregnancy are mimicked by taking artificial hormones. This is how some of the most effective methods of contraception, the deliberate prevention of pregnancy, disrupt the release of egg cells. Oral contraceptives or birth pills combine synthetic estrogen with progestin, a synthetic progesterone-like hormone.
Other hormonal contraceptives contain only progestin to cause a woman’s cervix to secrete thick mucus, preventing the entry of sperm; it also has the effect of decreasing the frequency of ovulation. Care and medical advice should be taken into consideration when taking these hormonal contraceptives as they both have harmful and beneficial side effects.
Other means of contraception involve surgery such as tubal ligation (removal of a section of the fallopian tubes and tying the ends to block the route of gametes) in females and vasectomy (cutting the vas deferens, preventing the sperm to reach the urethra) in males. Devices such as intrauterine devices (IUD) could also be placed by a healthcare provider within the uterus; there are also condoms that act as barriers and become more effective when used with spermicides.
The aforementioned methods carry different degrees of effectiveness and it is most obvious that the only completely effective method of birth control is abstinence.
Diseases of the Reproductive System
There are different means by which “pleasurable” activities such as intercourse can be risky to one’s health. Sexually transmitted infections (STIs), also called sexually transmitted diseases (STDs), are caused by pathogens that spread through sexual contact. Not all STIs are treated equally; those caused by bacteria, protozoa, and fungi are treated with medication while STIs from viruses cannot. Here is a list of some common STIs:
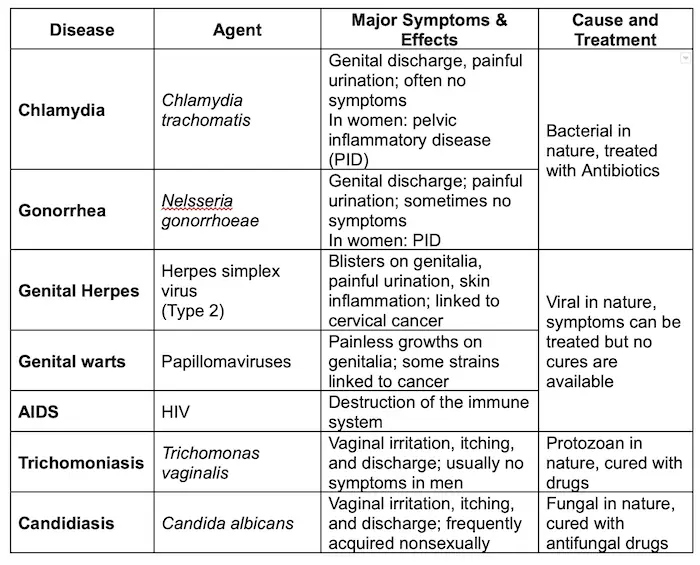
Many STIs can be effectively treated if addressed early. If left untreated, an STI may lead to long-term problems or even death. Anyone who is sexually active should have regular medical exams, be tested for STIs, and seek immediate help if any suspicious symptoms appear, even if they are mild.
The ultimate goal of the reproductive system is to bear the young that will pass on the genes and keep species alive. It all starts when the sperm joins the egg, a process which we will tackle next.
Embryonic Development

As soon as fertilization is successful, embryonic development begins. Fertilization combines haploid sets of chromosomes from two individuals and activates the egg by triggering metabolic changes that start embryonic development.
Among millions of sperms ejaculated, only one will be able to penetrate and fertilize the egg and add its unique set of genes to those of the egg, contributing to the next generation.
The sperm cell is streamlined to be able to swim through the woman’s reproductive system. It has a thick head that contains the haploid chromosomes, tipped by the acrosome, which contains enzymes that help the sperm enter the egg.
The middle section of a sperm cell contains the mitochondria which are able to absorb the nutrients provided by the semen in order to help the sperm move its tail. Much of a sperm’s energy is consumed by the time it reaches an egg but a successful sperm still has energy left to be able to penetrate the egg and deposit its nucleus in the egg’s cytoplasm.
A Closer Look at Fertilization
The process of fertilization begins as soon as there is contact between the sperm and egg. The moment a sperm hits the jelly coating of the egg, the acrosome releases enzymes to dissolve it. An extension of the sperm’s head penetrates the jelly coat and species-specific proteins bind to specific receptors on the egg. The sperm proceeds through the vitelline layer, and the sperm’s plasma membrane fuses with the egg. This fusion triggers a number of changes in the egg.
After the membranes fuse, the entire plasma membrane of the egg immediately becomes impenetrable to other sperm cells. Shortly after, the vitelline layer hardens and separates from the plasma membrane. The created space fills with water, and the vitelline layer becomes impenetrable to sperm. Meanwhile, the sperm’s nucleus enters and fuses with the egg’s nucleus.
An enormous series of growth and development will soon follow. DNA synthesis begins and cellular respiration speeds up. This also allows the egg to completely finish undergoing meiosis II. The sperm contributes only chromosomes to the zygote; the cytoplasm and all other organelles were provided by the egg.
We will now look and trace the development of a zygote into a new individual.
Embryonic Development in Animals
First Phase: Cleavage
Development begins with cleavage, a series of rapid cell divisions. After a zygote divides for the first time, it is called an embryo. The embryo does not enlarge significantly; instead, the number of cells doubles with each division, partitioning the cytoplasm into the many smaller cells.
As a result, each cell is much smaller than the original cell that formed the zygote. As cleavage continues, a fluid-filled cavity called the blastocoel forms in the center of the embryo. When cleavage is completed, there will be a hollow ball of cells called the blastula.
Cleavage makes two important contributions to early development: (1) It creates a multicellular embryo from a single-celled zygote; and (2) it is an organizing process, partitioning the blastula into developmental regions.
Identical twins come, at random, from a cell in the early embryo phase separating and “resetting” as if it were the original zygote and proceeding to development. On the other hand, fraternal twins (or nonidentical twins) occur from a different mechanism: when two separate eggs are fertilized in the same pregnancy.
Second Phase: Gastrulation
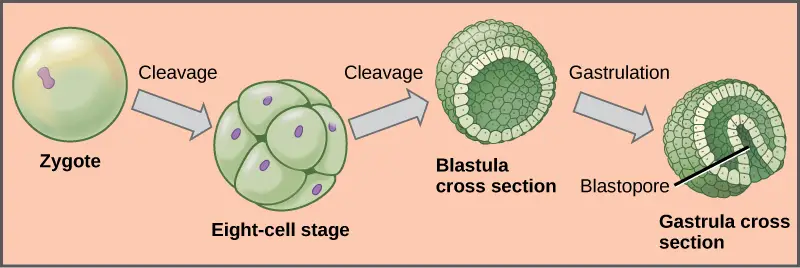
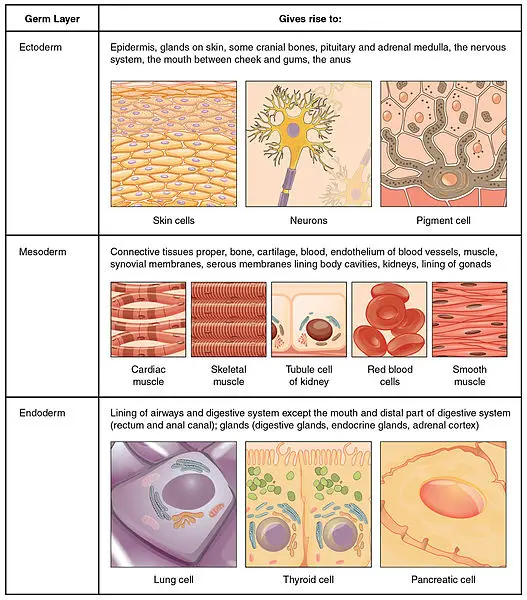
After cleavage, cellular division slows and groups of cells undergo gastrulation, where cells take up new locations that will allow the development or formation of the organs and tissues. As gastrulation proceeds, the embryo becomes a three-layered stage called a gastrula.
Here are the three layers of the gastrula and the organs (derivatives) they will form in a normal development:
| Layer (from outer to inner layer)Organs and Tissues They FormEctodermThe epidermis of the skin, the epithelial lining of mouth and rectum; sense receptors in the epidermis; cornea and lens of the eye; nervous systemMesodermSkeletal system; muscular system; circulatory system; excretory system; reproductive system (except gamete formation); dermis of the skin; lining of the body cavityEndodermThe epithelial lining of the digestive tract (except mouth and rectum); epithelial lining of the respiratory system; liver; pancreas; thyroid; parathyroids; thymus; lining of the urethra, urinary bladder, and reproductive system |
Gastrulation varies between species but the same general mechanisms drive the process in all species. A blastula will have regions of unequally sized cells. The cells toward one end, the animal pole, are smaller than the opposite end, the vegetal pole. During gastrulation, cells migrate to new positions that will form the three layers.
Gastrulation begins when the blastopore, a small grove, appears on one side of the blastula. Cells of the outer layer roll inward at the blastopore; the future endoderm surrounds a simple digestive cavity. Meanwhile, the cells that will form the ectoderm spread over more of the surface of the embryo, and the cells that will form the mesoderm begin to spread into a thin layer inside the embryo, forming a middle layer between the two.
By organizing the embryo into three layers, gastrulation sets the stage for shaping the animal. Cells in each layer will begin to differentiate into tissues and embryonic organs. An organ called the notochord will develop in the mesoderm while a structure that will become the hollow nerve cord is beginning to form in the ectoderm. The notochord is similar to cartilage and later in development, will allow the formation of the backbone. The notochord persists until birth but parts of it are present as disks of the adult spine.
A thickened region of ectoderm called the neural plate is destined to become the brain and spinal cord. From the neural plate, arises a pair of ectodermal ridges called neural folds. As the neural plate and folds develop, the neural plate rolls into a tube, which sinks beneath the surface of the embryo and is covered by an outer layer of ectoderm. The cells of the ectoderm fold inward, first elongating then becoming wedge-shaped. The result is a tube of ectoderm, the neural tube, which will become the brain and spinal cord.
Besides the neural tube and digestive cavity, other changes that develop are a series of internal ridges called somites, which are blocks of mesoderm that will give rise to segmental structures (repeating units like the vertebra), and a hollow space–the body cavity or coelom. The segmented body parts and the coelom are basic features of all chordates.
A key focus of this series of topics is to build from the simple structures developed by structurally “simpler” animals and apply them to the human body. As such, the next section will delve into how the zygote becomes a baby and the structures required to protect the development of the baby.
Overview of Human Development
Pregnancy or gestation is the carrying of developing young within the female reproductive system. Pregnancy starts at fertilization and continues until birth.
Fertilization, or conception in humans, occurs in the oviduct. Cleavage starts about 24 hours after fertilization and continues as the embryo moves down towards the uterus. A week after fertilization, the embryo reaches the uterus and cleavage has formed around 100 cells. The embryo is now a hollow sphere of cells called a blastocyst (mammal equivalent of a blastula).
The blastocyst has a fluid-filled cavity, an inner cell mass that will form the embryo, and an outer layer of cells called the trophoblast, which secretes enzymes that allow the implantation of the blastocyst into the uterine lining.
The trophoblast eventually forms part of the placenta, an organ that nourishes and protects the embryo and helps it dispose of its metabolic wastes. The placenta is made from both embryonic and maternal tissues. Three extraembryonic membranes, structures that support the embryo’s attachment to the mother, will develop from the embryo’s inner cell mass: the amnion, the yolk sac, and the chorion. A later membrane, the allantois, will develop as an extension of the yolk sac.
Roles of the Extraembryonic Membranes
The amnion will grow to enclose the embryo. Its cavity will be filled with fluid, which acts to enclose and protect the embryo. The amnion usually breaks just before childbirth, with the amniotic fluid leaving the mother’s body. Many anxiously expecting parents refer to this as the “water breaking,” and is usually taken as a sign to get to the hospital.
In birds and other reptiles, the yolk sac contains the yolk that provides nourishment to the developing young. In humans and other mammals, the yolk sac contains no yolk but will produce the embryo’s first blood cells that will migrate into the embryo.
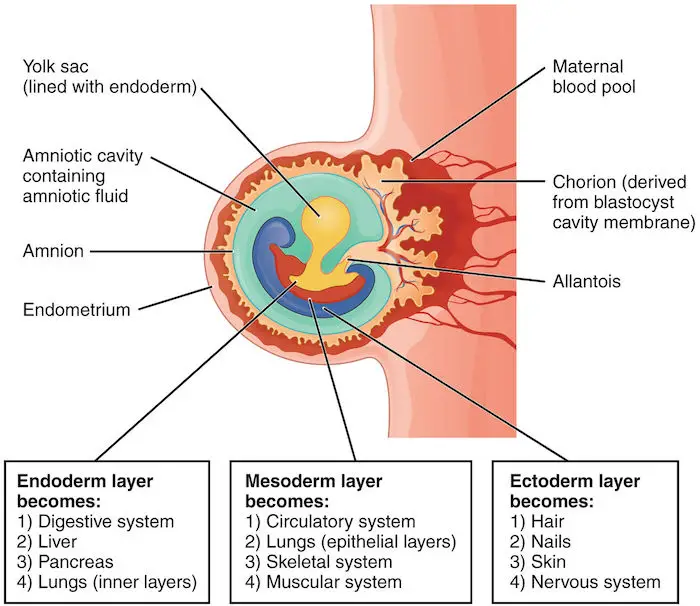
The allantois remains small in mammals. It will form part of the umbilical cord which acts as a mediator between mother and child. Additionally, it acts like the baby’s urinary bladder. In egg-laying animals, the allantois is larger and also functions in waste disposal.
The outermost membrane, the chorion, becomes part of the placenta and contains cells that secrete human chorionic gonadotropin (hCG). hCG, as mentioned before, maintains the level of estrogen and progesterone which then maintains the corpus luteum. Bumpy outgrowths from the chorion, called chorionic villi, contain mesoderm and will form embryonic blood vessels.
By this time, the placenta is fully developed. Made of maternal and embryonic tissues, the placenta is a vital organ for mediating the exchange between mother and child.
Human Pregnancy
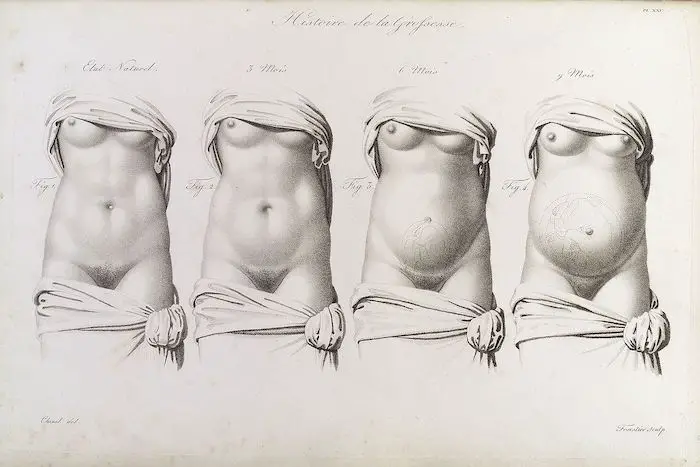
Pregnancy can be divided into three trimesters, each lasting about three months. In the first trimester, the most radical changes occur for both mother and embryo. During this time, the embryo is very vulnerable to damage made from the intake of alcohol, drugs, cigarettes, and the like which can lead to birth defects and miscarriages.
During the second trimester, the fetus continues to grow and will develop more human-like features, though the change is not as dramatic as the first trimester. The fetus will be able to open its eyes, the teeth are forming, and the bones will harden. The placenta will secrete progesterone (the corpus luteum stops secreting progesterone), which helps maintain it. Simultaneously, the placenta stops secreting hCG, and the corpus luteum degenerates.
In the third trimester, the fetus grows and strengthens in order to survive outside the protective environment of the uterus. As the fetus grows, the uterus expands and squeezes the mother’s abdominal organs, leading to frequent urination, digestive troubles, and backaches.
After the trimesters and normal development of the baby, the series of events that will lead to the infant expelling from the uterus is called labor. It can be divided into three stages and hormones and other signals are needed to properly deliver the baby.
The first stage, titillation, is the onset of labor until the cervix becomes widest. It is the longest stage of labor, lasting 6-12 hours or longer. The period after is the expulsion stage where the infant is forced down and out of the uterus and vagina. The afterbirth is the final stage of delivery, during which the umbilical cord is cut and the placenta is delivered.
We mentioned earlier that the brain and different nerves coordinate the various complex mechanisms in the body. It is now time to take a deeper look into this very important organ system next.
Next topic: Nervous System
Previous topic: Endocrine System
Return to the main article: Animal Form and Functions (Overview)
Download Article in PDF Format
Test Yourself!
1. Practice Questions [PDF Download]
2. Answer Key [PDF Download]
Copyright Notice
All materials contained on this site are protected by the Republic of the Philippines copyright law and may not be reproduced, distributed, transmitted, displayed, published, or broadcast without the prior written permission of filipiknow.net or in the case of third party materials, the owner of that content. You may not alter or remove any trademark, copyright, or other notice from copies of the content. Be warned that we have already reported and helped terminate several websites and YouTube channels for blatantly stealing our content. If you wish to use filipiknow.net content for commercial purposes, such as for content syndication, etc., please contact us at legal(at)filipiknow(dot)net
